What I enjoy most about my job are the stories. Tales of resilience, trudging through struggle and persistence that is awe-inspiring. Tales of celebration and transformation allowing lightness to be just as present as the heaviness. To have the privilege to bear witness to the rawness of life—the vulnerability that may have never been spoken outside the walls of my office, is an opportunity I try not to take for granted. While diplomas hang on my office wall constituting some level of due diligence for my job, my most meaningful work does not come from a textbook or fancy training, but in the simple act of providing a platform for somebody to feel seen, heard, and validated.
I have been asked many times why I have chosen this line of work. Put simply, a mental health provider is not for those who desire logic and certainty. It is a field that demands a draw to creativity, at least a bit of proclivity for drama, and a sustained fascination for what lies between point A and point B in a person’s life. What are the layers and circumstances behind action and behavior? But perhaps most of all, being a mental health provider demands an appreciation for mystery, ambiguity, and uncertainty.
Despite attempts for algorithms and treatment protocols throughout the years, the field of psychiatry and mental health has long been on shifting sand. The first edition of the Diagnostic Statistical Manual of Mental Disorders was released in 1952 and to date, there have been eight revisions published by an appointed committee of reportedly well-regarded experts tasked with establishing what has become a bit of a subjective and culturally informed bible to the mental health profession.
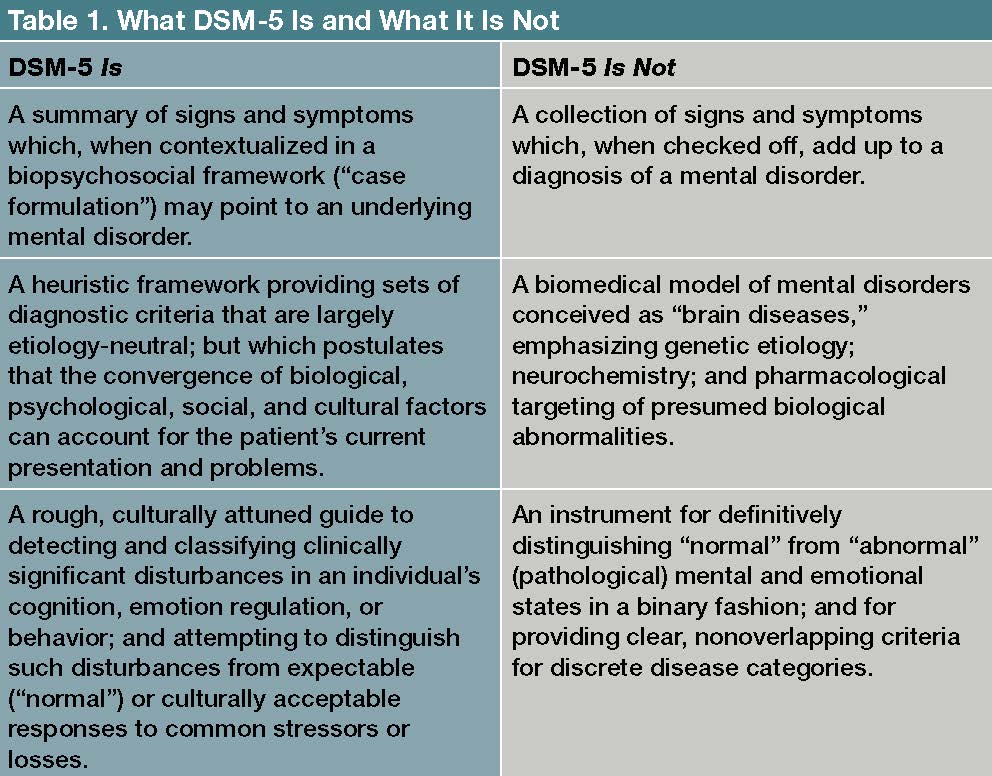
The diagnoses found in what is currently the DSM-5-TR have provided a sense of clarity and validation for many and have provided targets for specific treatments, but for most of these so-called pathological conditions, there is little scientific basis constituting them as anything more than well-thought-out descriptions of generally to be expected sequelae. The DSM has attempted to universally categorize and define the vastness of human emotion, which at its essence is deeply personal, full of paradox, interconnected, and strongly intertwined with context and circumstance. Per my opinion, we have to take it all with a grain of salt.
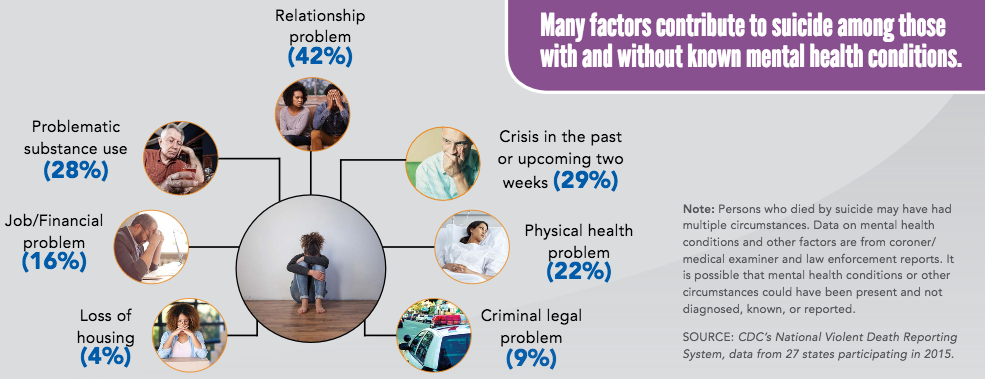
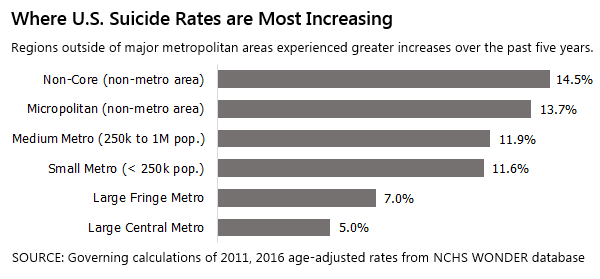
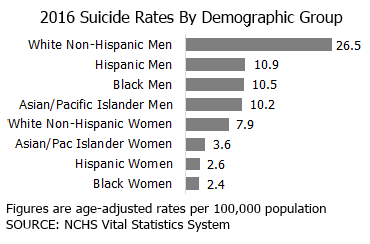
Alongside the subjectivity of mental health diagnoses, are widely accepted theories that depression concurrent with other mental health diagnoses constitutes an “imbalance in the brain”. This has historically referred to an imbalance or deficiency in the monoamine neurotransmitters (serotonin, dopamine, & norepinephrine). This monoamine hypothesis has served as the primary catalyst for extensive pharmaceutical campaigns promising the latest and greatest pharmaceutical agents to “restore” such imbalances. Yes, sometimes medications can be helpful and even lifesaving, but despite fancy names and multi-million-dollar ad campaigns, the extent of progress against rising rates of depression, suicide, and substance use, ought to be questioned. Extensive peer-reviewed studies have suggested that only about a third of antidepressant users will appreciate some level of improvement.
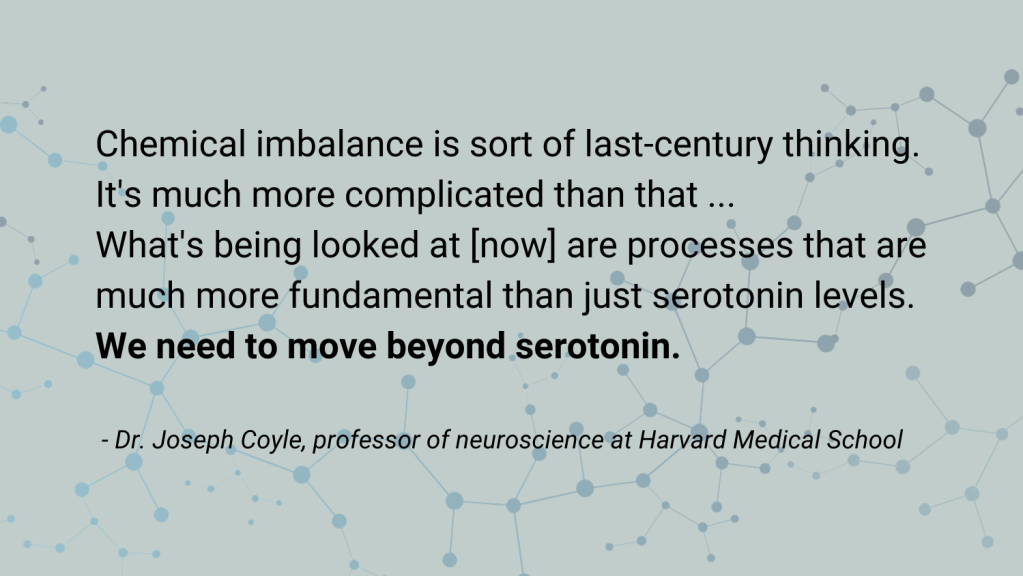
A recent extensive review conducted by University College London scientists and published in Molecular Psychiatry (July 2022) scrutinized the leading hypothesis that depression (and implicitly other mental health conditions) is a consequence of an imbalance in serotonin. In a thorough review of tens of thousands of subjects, researchers found no significant difference in serotonin levels among depressed versus healthy subjects. This shakes the foundation supporting the use of antidepressants predicated on the seemingly debunked monoamine hypothesis. With antidepressant use sharply on the rise in recent years for both adults and children, it makes one wonder how such a precarious theory became so widely accepted. And yet, I suppose that is what pharmaceutical companies do best…followed by insurance companies. While antidepressants should not be completely disregarded, the study further emphasizes the need for a holistic, contextually informed approach to mental health concerns.
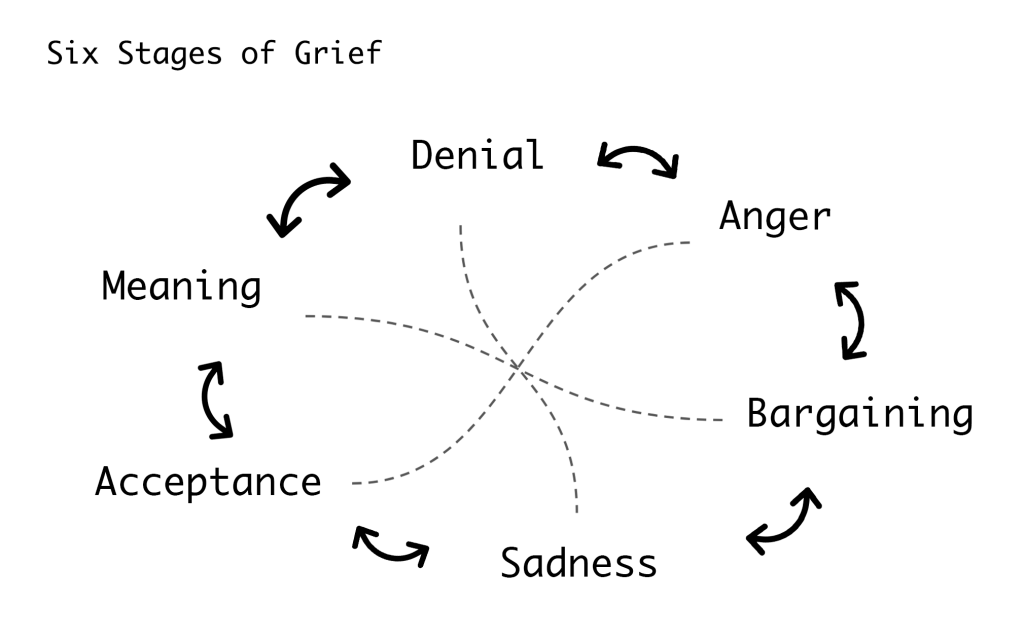
The goal of emotional wellness should not be to avoid pain and sadness, but to embrace the inevitability of struggle balanced with the hope to cultivate moments of joy, gratitude, and connection. It is a quest that is undoubtedly easier for those with resources and supports and has also become difficult when up against our mainstream culture that exploits insecurities, fear tactics, time scarcity, and has cast a long shadow of existential gloom for many of us. Simultaneously, the prevailing message of mainstream mental health is that accommodations ought to be made per our discomforts perpetuating the idea that we are entitled to the path of least resistance. Our tolerance for struggle has dwindled and our resilience has faltered with it.
Regardless of nostalgia for better times, the world has always had its dark spots. In times past, we had more distance from it all as we awaited the daily newspaper or a phone call. Now, exposure and susceptibility to vicarious trauma is only one click away and as immediate as ever. Adults and parents seeking to buffer children from danger may be unintentionally robbing opportunities for resilience-building and transferring their own anxieties. Children are less likely to drive, get a summer job, date, do chores, and communicate face-to-face. On the outside they are growing up slower, but as soon as they pick up their device, they are confronted with a slew of emotionally charged topics that overwhelm even the most emotionally mature—divisive politics, bullying, climate change, war, death, mass shootings…who wouldn’t be anxious?
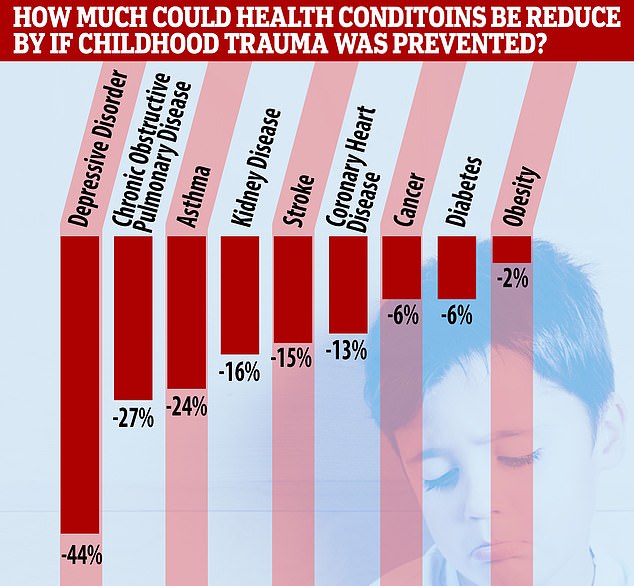
Uncomfortable emotions are part of the human experience and can be just as informative as they can be problematic. Depression, anxiety, poor focus, burnout, and other common complaints these days cannot be attributed solely to an imbalance, or a subjective description written in a manual. Depression and many other mental health diagnoses remain complex, perhaps not always a “disorder”, often rooted in trauma, and may tell us more about the angst and urgency of mainstream culture than about actual pathology.
Relying on arbitrary theories to explain emotional distress can minimize our responsibility to ourselves as we contemplate lifestyle and connection, but also to our neighbors as we contemplate policy and social reforms. Therapy and pharmaceuticals only go so far when the feelings of environmental safety and stability are frequently in jeopardy. Strengthening our collective emotional wellness demands advocacy, an acknowledgment of privilege, and innovation- a conversation we can all contribute to.
Thank you for listening, everyone.

With gratitude,
Audry Van Houweling, Owner, She Soars Psychiatry, LLC
Sisters & Silverton, Oregon