Here’s to my first blog post ever! After pondering what I wanted to say, I felt compelled to write about something we all share…trauma. Uplifting? Not so much, but trauma and stress is often the launching pad from which so many chronic conditions arise and it seems fitting that we start with foundations.
That’s right ladies (and yes, men too)- I have a theory that we are all traumatized. If you you have somehow escaped trauma, congratulations, and please share your secrets. Before you call me Debbie Downer and switch to your favorite cooking blog, keep reading- it’s important.
Within conventional psychiatry and psychology, when the burden of trauma elicits a certain set of criteria from a person, they may be diagnosed with post-traumatic stress disorder (PTSD). I personally have a bit of a beef with labels we use in mental health and do not like the word “disorder”. I find it limiting and disempowering.
As I will explain a bit in this post and more extensively in the future, the symptoms that define PTSD may be counterproductive in certain situations, but are rooted in our evolution and survival instincts.
What is trauma? In my assessment, trauma can be characterized as anytime we have a perceived sense of helplessness or loss of control. It is something that has caused harm or has the perceived potential to cause harm. It can be a physical form- a person, a place, an object, or it can be a collection of thoughts, memories, nightmares. Trauma is not necessarily what happened to us, but the effect it has upon us.
Let’s consider some examples. Have you ever been in a car accident? Did you know motor vehicle accidents are the number one cause of “PTSD”? I bet you can remember certain details…perhaps it happened at a particular intersection or stretch of road, perhaps you had a certain song on the radio at the time, or you can remember the time of day, or the weather.
Have you ever felt belittled, harassed, talked down to, discriminated against? Most of us- especially women and girls have had this experience at one time or another. Maybe it was a coworker, a significant other, a stranger on the street, or a family member. Or maybe you are a survivor of sexual assault or abuse…or maybe you witnessed somebody else’s trauma… or maybe you heard about something scary on the news…you see, given all the possibilities, it is hard to imagine anyone would not be traumatized.
Do you notice the discomfort and vulnerability when walking alone? Maybe you carry pepper spray, a knife, or even a gun. Perhaps you have become really good at assessing the scene, looking over your shoulder, looking for signs of danger. Do you find yourself feeling inferior or intimidated around others (particularly men) even when you stand for equality and you know this should not be? Is it hard to look people in the eye, speak up for yourself, be assertive? You may not have actually experienced an attack or harassment, but by simply being privy to stories in the media or from someone you know, you may adopt certain behaviors in response to a potentially traumatic situation.
And then there’s the trauma of not feeling good enough and the negative self-talk that comes with it. For so many of us, we have a constant buzz within ourselves to look a certain way, meet societal expectations, lose the weight, perform in our jobs, buy the right clothes, appease our families, religious organizations, significant others, children… and all the while do it with a smile, because you know, we have to have those Facebook posts just right.
Our society breeds dissatisfaction and it seems that us women & girls are particularly susceptible to this near-constant, hypervigilant mindset of what must I do to be better? What must I do to be on par with everyone else? Well, maybe I should get some pointers from Facebook, Instagram, etc…see how I measure up…but wait, that did not make me feel any better! This hypervigilance can be traumatic in itself as it creates the ongoing need to feel more and more in control of our appearance, reputation, and what we portray to the world. Unfortunately, this race has no finish line and we often exhaust ourselves trying to find it.
Trust me, I am entirely guilty of this- hard not to be, right? Type A personality, perfectionist, ambitious, afraid to settle…yup, all worthy descriptions of who I am. I do not have a pedestal and even if I did, I would still have my self-doubts…
Trauma is like throwing a stone into the water. There is the initial impact, but then there are the ripples…
Let’s go back to a time when you felt belittled or talked down to. If this has happened a lot in your life, you might find yourself often defensive and feel as though you have something to prove. Can you remember the person that did this to you? I imagine you remember them well. Can you remember where you were when it took place?
Can you remember the feelings of fear, anger, shame…? Have you met others that reminded you of that person, that place, or maybe you have gone further to generalize your experience to being associated with an entire group of people. Ripples…trauma builds on itself. The original trigger multiplies into more triggers and then more triggers from secondary triggers and so on.
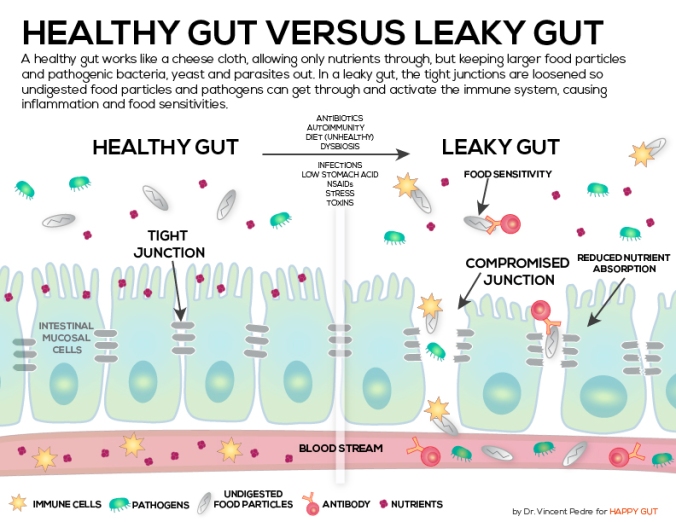
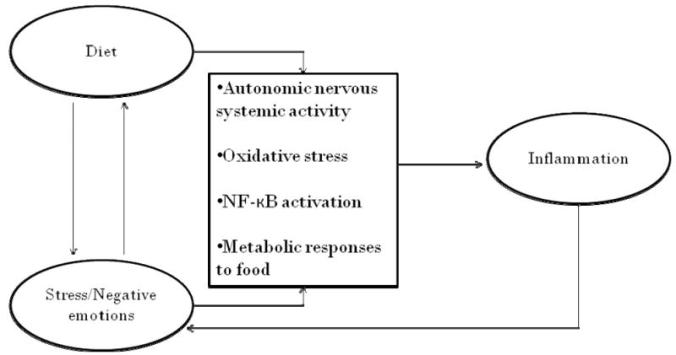
Trauma is not something that hides out in the brain. It elicits reactions throughout every system in your body from your head to your toes. Every thought and emotion positive or negative has an associated chemical reaction that is communicated throughout our body. We will go more into this later.
Ever feel achy, sick, fatigued, nauseated in the midst of stress? Yup, a few of the not so uncommon reactions.
Going back to evolution- when we are faced with something potentially harmful or life-threatening, our natural reaction is to fight or flight. Basic survival instincts.
While this can be really helpful when you are being chased by a bear, some of us (actually a lot of us) find ourselves in a perpetual state of fight or flight driven by actual or imagined fears, threats, or circumstances. It is important to remember that events or situations that may not be perceived as “traumatic” can cause this same reaction. Having a baby, starting a new job, moving, starting a relationship are a few examples. We might feel buzzed at first- energized, enthused, but then the surge of adrenaline and other stress hormones may not sustain themselves and we feel the burden of fatigue, burn out, apathy, sadness, and even despair.
Some of us in the midst of feeling the lull, may seek out even more exciting or risky ventures that may spike our interests and adrenaline levels for a while longer before we again fall back and the cycle continues. Addictions work this way too.
You see, some of us can become so familiarized with trauma and chaos that it becomes part of our identity…our modus operandi, our comfort zone, our ego. Some of us may be conscious of this while some of us have not yet recognized it. Do you take pride in being able to juggle so many balls at once? Do you have a silent pride in being there for somebody who may be abusive, but you feel you are the only one that can help? Do you find yourself attracted to gossip and drama? Perhaps you like the thrill of a challenge and have difficulty with stillness, quiet, and slowness? Do you like danger, risk-taking, pushing the envelope? Is it harder to receive love and care then to extend it to others? If you are like a lot of us, the answer is yes, yes, and yes.
How do you identify or label yourself? Might it be that how we define ourselves and the labels we assign to who we are can also cause pain and perhaps perpetuate trauma? If we are too rigid with our expectations for ourselves and keep ourselves in a box, we are likely to be disappointed.
If we are all traumatized, we are also all on a spectrum. Some of us are in the midst of trauma right now. Some of us are struggling to overcome memories of trauma. Some of us are being overwhelmed with the news of our world today.
Ask yourself how you perceive yourself in the midst of the trauma past or present? What is your role? Victim, survivor, witness, standing on the sidelines? How do you also label the person, place, event, or thought process that perpetuated the trauma?
Language is powerful. Remember that feelings are real, but they are not always true.
Medication, supplements, fitness, and lab testing all certainly have their merits in supporting wellness, but true vitality and contentment often lies in how we perceive ourselves and others around us. It is the process of learning to trust ourselves and in doing so, be able to extend trust to others.
Be careful how you perceive yourself, how you label yourself. Be careful not to let yourself be defined with too much rigidity. Embrace fluidity. Be kind to yourself and give yourself grace. Recognize that you are not alone.
I am fascinated with the concept of resilience in the midst of trauma…I would love to hear from you how you main resilient? What keeps you grounded? Please share!
In future posts we will be discussing the physiological impacts trauma has throughout our bodies and steps we can take to restore vitality and stay grounded in the midst of our complex world! So stay tuned!
As always find out more about us at http://www.shesoarspsych.com
Be well,
Audry Van Houweling, PMHNP-BC