I have an unusually strong affinity for small towns. Some people find more energy and excitement in the big city, but to me there is an undeniable allure and richness within the layers, roots, stories, and secrets of generations past that define small town America. I am intrigued by both the triumphs and woes that give a place identity and how this influences the collective consciousness of its residents.
This collective consciousness or energy is much more palpable in a small town. Ripples of change are felt more acutely- more intimately. It is as if you would compare a pebble being tossed in a fish bowl with a pebble being tossed in a lake.
These ripples carry energy- both positive and negative.
Ripples carrying the anticipation of the local parade. The relief from the local festival boosting business. The celebration of the Friday night football victory. The pride of this year’s graduating class. The excitement of a new store or coffee shop coming to town.

Ripples also carrying the unease when business gets slow and jobs dissipate. The grief that permeates when somebody passes on. The helplessness of addiction that can swallow communities alive. The desperation felt at Sandy Hook, Sutherland Springs, Roseburg, Blacksburg, and too many others.
Even events that may seem small and commonplace- marriage, divorce, a child’s struggle, illness, financial strife, and more can have significant impacts in a small town as one individual can have so many interconnections with others.
The communities where I currently practice in Oregon- Sisters & Silverton, have been fortunate to enjoy recent economic prosperity, growth, and are both known as desirable destinations. Working in mental health you learn to appreciate stability, but also to look beyond the charm. You learn about grief, bullying, scandal, loss, and family dysfunction with roots dating all the way back to the Oregon Trail.

Trauma in a small town can be both collective in that it is felt by many whether or not they directly experienced the event and/or intergenerational in that the pain can be transferred from one generation to the next.
The intricacies and dynamics of all these interconnections can also create a level of stigma as asking for help can seem too risky or too vulnerable. There may be fear of gossip, a breach of confidentiality, or simply being able to find someone to talk to without bias.
The beauty of small towns however is that in this web of interconnections, deeply rooted generations, and tight knit community is also power. Small acts of kindness are not so small. Creating space for vulnerability and authenticity in our schools, places of worship, and social gatherings can have far reaching impacts. Seeking common ground rather than reinforcing divisions can create a net of safety and acceptance. Valuing community instead of self-reliance. Creating dialogue about the hard stuff- depression, anxiety, grief, addiction, trauma, suicide, and shame can take someone from a place of isolation to empowerment.
Albeit perhaps for selfish reasons, my role as a mental health provider seems to have more significance in a small town when an individual’s progress seems to have more immediate impacts on their family, workplace, school, and ultimately, the community.
In summary, while the place in which we live has an impact on our identify and self-concept, it is also our actions and beliefs that help define and transform a place. In the meantime, I continue to enjoy the great privilege of being part of the small-town experience…and dropping my pebble in the fishbowl.
With gratitude,
Audry Van Houweling, PMHNP-BC, Owner & Founder, She Soars Psychiatry, LLC




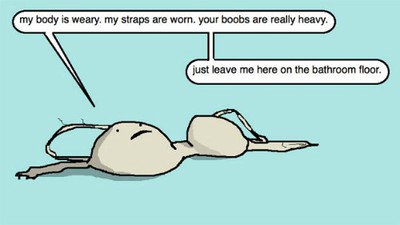 I worked at “VS” on and off for the next five years through my undergraduate days. The wages did not get much better and the hours were still sporadic, but in addition to feeling suave in my black blazer and heels, I learned a few things about customer service. Certainly, the art of customer service could have been learned elsewhere, but when you deal with women, breasts, bra size, insecurity, and vulnerability, you better be careful with your words, be a good listener, personalize each client’s experience, and treat every woman (and the occasional man) with respect.
I worked at “VS” on and off for the next five years through my undergraduate days. The wages did not get much better and the hours were still sporadic, but in addition to feeling suave in my black blazer and heels, I learned a few things about customer service. Certainly, the art of customer service could have been learned elsewhere, but when you deal with women, breasts, bra size, insecurity, and vulnerability, you better be careful with your words, be a good listener, personalize each client’s experience, and treat every woman (and the occasional man) with respect.






