Oh hormones…it seems you are my worst enemy and my best friend depending on the day. Sometimes you make me happy, sometimes you make me sad, and sometimes you make my husband fear you. Ladies, I think we can all relate.

How many times have people accused you of being “hormonal”? Feels a bit sexist, right? Was it your significant other as is often typical? I think it’s about time as women that we take this term back- reclaim it. My response is, “Well yes, I am hormonal and in fact, my hormones probably made you attracted to me in the first place. Thank you very much”.

As women we experience dynamic hormone transitions throughout our lives. Whether it is our monthly cycle that may be predictable or highly unpredictable, pregnancy, lactation, and/or menopause, we have all experienced the force of our body’s messengers. Sometimes these changes and transitions are rejuvenating, sometimes just tolerable, sometimes comical, but sometimes they can cause serious disruptions in our mood and overall vitality.

In conventional psychiatry, there is an acknowledgment that hormones may play a role in emotional wellness, yet it remains rare that hormone levels and function are actually tested for and considered with making treatment decisions. Unfortunately, too often psychotropic medications such as antidepressants or mood stabilizers are prescribed without a second thought to addressing hormone balance. Clients may meet every criterion for clinical major depressive disorder and per recommendations, would be a “good candidate” for an antidepressant, and yet lab tests may reveal significant hormone imbalances such as thyroid dysfunction, which when corrected remedies the depressive symptoms. Go figure!
At She Soars Psychiatry, we focus on hormones that we feel are most implicated in influencing your emotional wellness.
For the sake of maintaining your focus, I will not get too wordy with the science, but if there is a take home message, please consider getting your hormones checked before jumping to the conclusion that you have a “mood disorder”. Here are some noteworthy hormones worth consideration.
Noteworthy hormones for women:
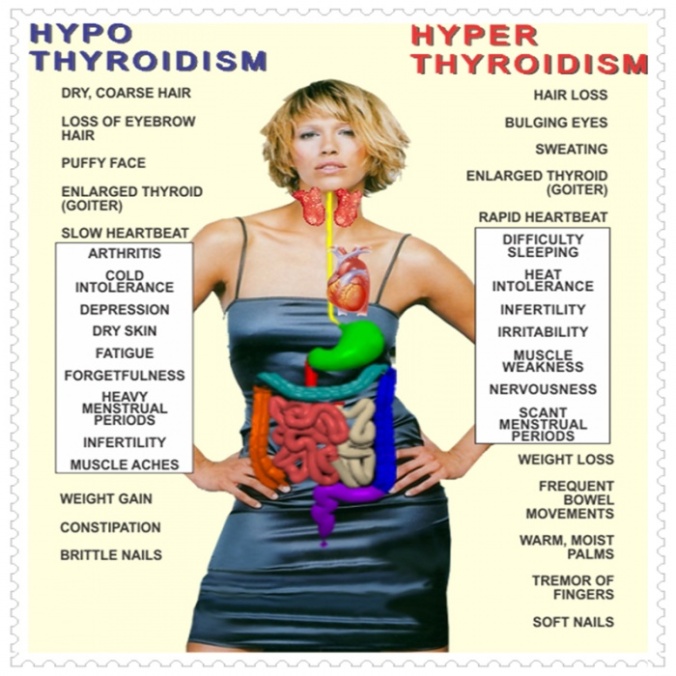
Thyroid: Thyroid function is critical to maintaining emotional wellness. Dysfunction may be caused by multiple mechanisms including autoimmune disease. Hyperthyroidism (producing too much thyroid hormone) can cause insomnia, panic attacks, irritability, heat intolerance, and more. Hypothyroidism (producing too little thyroid hormone) can cause fatigue, depression, cold intolerance, weight gain, and foggy thinking. Women can be particularly susceptible to thyroid dysfunction following childbirth, which needs to be considered if postpartum mood symptoms are experienced.
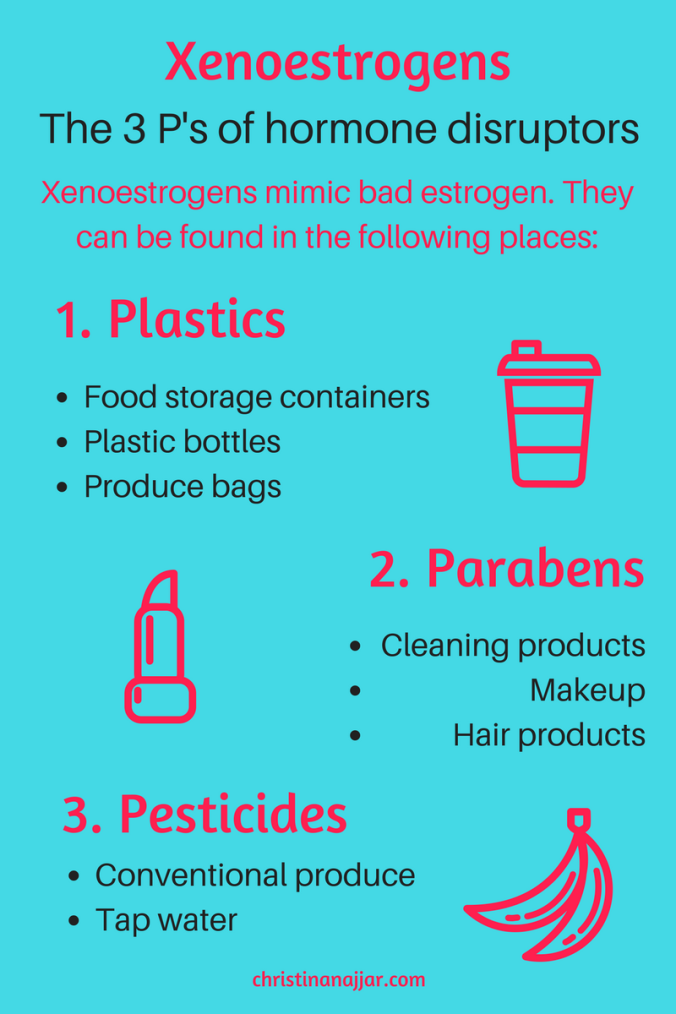
Sex hormones: An imbalance between estrogen and progesterone can lead to multiple mood symptoms. Estrogen dominance or excess can cause symptoms of both depression and anxiety along with progesterone deficiency (the two often go hand in hand). Testosterone is also important for women and plays a role in facilitating motivation, sex drive, and energy levels. Our environment is full of xenoestrogens (estrogen mimicking compounds), which can cause further hormone disruption. Sex hormone balance should be particularly considered in women on oral contraceptives, women experiencing pre-menstrual mood changes, women with endometriosis, polycystic ovarian syndrome, uterine fibroids, and women in the peri-menopause and menopause stages.
Adrenals & HPA axis function: This is a big topic and one we will explore further in detail. Essentially, your adrenals and HPA (hypothalamic-pituitary-adrenal axis) are an intimate part of your stress response. It all starts in your brain with the hypothalamus, which assesses internal and external information and then communicates with another very important part of your brain, the pituitary gland. When stressed, the adrenal glands (which sit on top of your kidneys) release both norepinephrine/epinephrine and glucocorticoids (cortisol). Many of you may have heard of cortisol and how chronically elevated levels of cortisol may be associated with inflammation, blood sugar instability, weight gain, and depression. In cases where stress is not alleviated such as post-traumatic stress disorder, cortisol levels may actually be depleted and cause symptoms of burn out, chronic fatigue, a lack of motivation, and even autoimmune conditions.

Hypothalamic-Pituitary-Adrenal Axis
The good news is that many of these hormones can be tested and there are practical and non-invasive steps you can take to restore hormone balance and vitality!
In the end, our hormones are amazing, yet delicate messengers that deserve the utmost respect for how they keep us feeling motivated, passionate, desirable, confident, and strong. They allow us to birth children, feed our children, run from danger, sleep well at night, and get up the next day ready to go at it again. So, no matter many times they have been your scapegoat or nemesis, they do deserve our praise.

Audry Van Houweling, Owner & Founder, She Soars Psychiatry, LLC
Wishing you balance and dynamism!
With gratitude,
Audry Van Houweling, PMHNP-BC, HNFM certified, DONA trained postpartum doula
Owner & Founder She Soars Psychiatry, LLC. Holistic Psychiatry & Wellness for Women & Girls.